The Employee Benefits Security Administration (EBSA) has posted a 10-page instruction book that explains how the new association health plan (AHP) regulations are supposed to work.
EBSA officials wrote the guide to explain what an AHP is, discuss what the new AHP regulations, and give answers to frequently asked questions about the new AHP regulations.
Some health insurance industry policy watchers have questioned whether the new AHP rules will be flexible enough to encourage widespread use of AHPs.
But EBSA officials are hoping the new AHP rules will help more small employers offer health benefits.
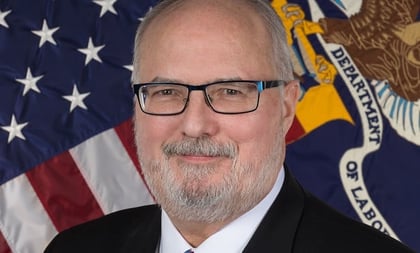
“Expanding access to AHPs creates a path to affordable health coverage for millions of American workers and their families,” Preston Rutledge, the head of EBSA, said in a statement about the new AHP regulations.
(Related: Trump’s Association Health Plans Will Be Like Big Employer Plans: DOL)
A copy of the AHP compliance guide is available here.
What is an AHP?
An AHP is a group for employers that want to team up to buy health coverage.
Under federal law, employers have been able to join together to form multi-state AHPs all along. But, in practice, rules for multi-state AHPs have been so rigid that most AHPs have operated in just one state.
The administration of President Donald Trump moved to expand use of AHPs this summer, by releasing regulations that let any eligible group offer an AHP for employers in a metropolitan area, even if the metropolitan area extends into two or three states.
The new regulations also let an AHP offer coverage to some or all employers in a designated trade or industry group nationwide, and they let an AHP offer coverage to self-employed people who have no employees.
Before, the rules for the kinds of employers a multi-state AHP could serve were much narrower.
What are some key AHP regulation effective dates?
Associations have been able to start fully insured AHPs under the new regulations since Sept. 1.








 October 03, 2018 at 05:32 PM
October 03, 2018 at 05:32 PM